This blog more focus about Bladder pain syndrome, Bladder pain, Reproductive system, Bladder cancer treatment, Interstitial cystitis.
For women suffering from bladder discomfort, an infection is commonly blamed, although it is not the sole culprit.
If your bladder is causing you to experience pain or pressure in your pelvic region or lower abdomen, this might indicate a serious health issue.
Bladder pain syndrome discomfort may indicate anything from a mild infection to a major medical disease, such as cancer.
Bladder pain syndrome range from soreness in the lower abdomen to burning during urination.
One piece of encouraging information is that bladder cancer is a difficult illness to diagnose, especially in females.
According to the American Cancer Society, it is anticipated that more than 82,000 people in the United States will be diagnosed with bladder cancer in the year 2023, with more than a quarter of those newly diagnosed cases being female.
However, this does not imply that you should disregard any pain or pressure in your pelvis or lower belly that your bladder might be causing.
The symptoms might still be indicative of a significant health condition. How can you determine if the discomfort is bothersome or suggests a benign condition?
NazemaY. Siddiqui, MD, an associate professor of obstetrics and gynecology at Duke University School of Medicine in Durham,
North Carolina, recommends paying special attention to your other symptoms, particularly if you have runny urine and soreness in your bladder.
Please Read This Great Info easy-way-to-understand-imposter-syndrome
The following conditions might cause bladder discomfort-Bladder pain syndrome

However, pelvic pain from gynecologic diseases may cause bladder discomfort. Certain gastrointestinal symptoms may also cause discomfort in or around the bladder.
“The advice that Dr. Siddiqui gives to ladies who are experiencing discomfort in their bladders is to seek medical attention. Land infections are more common in women.
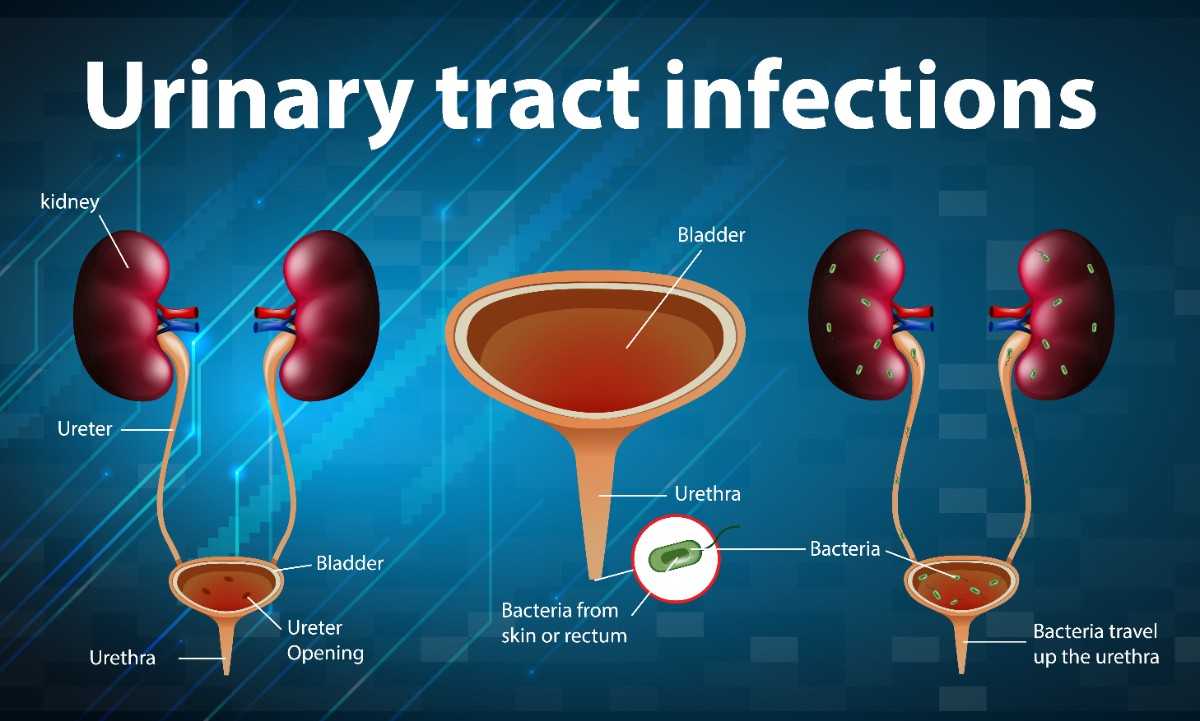
Urinary land infections (UTIs), also known as bladder infections, affect women more commonly than males, and the reason is simple deconstruction.
The urethra of a woman is located near areas that contain natural germs, such as the vagina and the anus. The NIDDK also notes that it is shorter than a male urethra, which is a bit of a bummer.
An infection of the urinary tract (UTI) may strike at any moment; it affects over 50% of women.
The Urology Care Foundation reports that younger women are more likely to obtain these infections as a consequence of sexual activity.
Still, older women are more likely to have urinary tract infections (UTIs) after menopause, which is characterized by a decrease in vaginal estrogen levels, than younger women.
Bladder pain syndrome –
Estrogen influences urinary tract health, and after menopause, the vaginal towel thins, leaving it more susceptible to infection.
According to 2019 research published in Remedial Advances in Urology, the UTI rate in women over 65 is double that of the general female population.
The same study found that a high rate of UTIs occurred with the peak of sexual exertion, which is typically between ages 18 and 39.
Bladder discomfort, as well as frequent and painful urination, are typical symptoms of UTIs in young women.
Bladder pain syndrome in older women might vary, often including stomach pains, abdomen pain, weariness, and weakness.
According to the NIDDK, Bladder pain syndrome , medications such as nitrofurantoin (Macrobid), trimethoprim/sulfamethoxazole (Bactrim), and fosfomycin (Monurol) may typically clear up a urinary tract infection.
Although an infection may resolve without treatment, antibiotics help hasten healing and quickly eliminate unpleasant symptoms.
Drinking plenty of water and peeing often will also help to cure the infection and relieve your pain.
Please Read This Great Info birth-control-pills-or-birth-control-with-low-estrogen
Interstitial cystitis
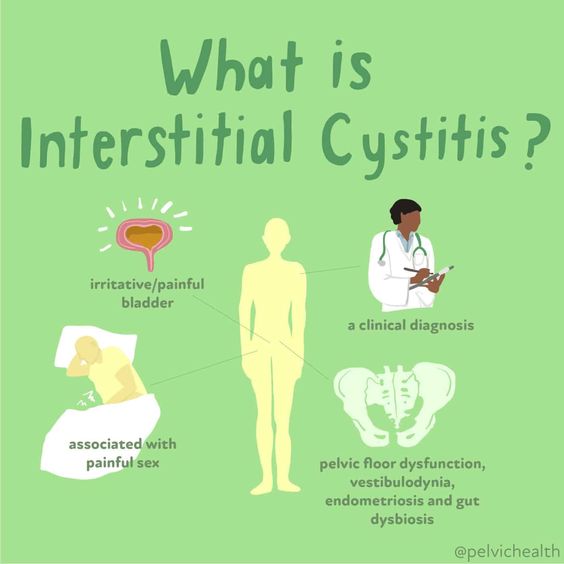
causes pelvic discomfort for almost three million American women, according to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
Inflammation and irritation of the bladder walls define this illness.”Interstitial cystitis is an austere shape of bladder pain pattern,” explains Siddiqui.
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), the level of pain it produces in the bladder may range from moderate to severe.
One of the Bladder pain syndrome of the condition is a patient has an intense need to urinate every few minutes.
According to the Mayo Clinic, this sensation may occur up to 60 times each day, including incontinence after urination.
A further indication is that the underlying cause is interstitial cystitis. Most of the time, menstruation makes the pain in the bladder worse.
A urinary tract infection does not cause interstitial cystitis; however, your symptoms may become more severe if you already have interstitial cystitis and then get a UTI.
While the reason is unknown, according to the NIDDK, some events or procurators induce flashes in Bladder pain syndrome.
These include pressure, dietary changes, disinclinations, and the use of certain medications, among other consequences.
The only way to treat interstitial cystitis is to slowly fill the bladder with fluid using a technique called embroidering,
take vocal drugs such as tricyclic antidepressants, antihistamines, and pentosan polysulfate sodium (Elmiron),
do physical therapy, and use an electrical Whim-Whams stimulation device to ease pain by sending mild impulses to jitters in the opposite direction.
In severe situations Bladder pain syndrome where other therapies have failed, surgery may be a possibility.
Please Read This Great Info five-things-to-know-about-melatonin-for-kids
Your Reproductive System- Bladder pain syndrome
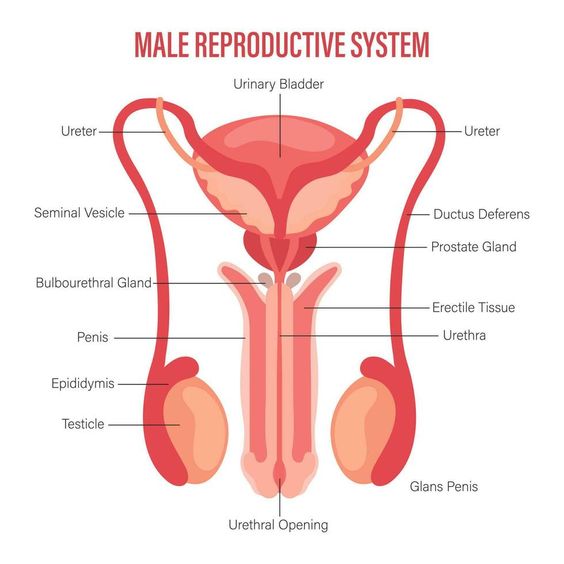
According to Karl Luber, MD, a urogynecologist and the creator of the womanish pelvic drug and reconstructive surgery rapport program at UCSD-Kaiser Permanente in San Diego, weakening of the vaginal face may be the cause of bladder discomfort in women.
“This is called atrophy, and it’s most common when menopause (or perimenopause) deprives the napkins girding the vagina of estrogen,” Bladder pain syndrome according to his explanation.
When estrogen levels drop, vaginal napkins compress and become thin. While vocal estrogen is ineffective, a vaginal estrogen cream, Bladder pain syndrome, may alleviate discomfort.
Some of these medications, like Premarin and Estrace, are only available via croaker tradition, although other undesirable choices exist.
Typically, they are used daily for one to three weeks, then utilized once a week afterward.
According to Dr. Luber, talking with your croaker about bladder pain and discomfort will help pinpoint where the problem resides.
Cancer is rare, yet it is nonetheless life-threatening – Reproductive system.
While bladder cancer is delicate, particularly in women, it is more likely to be identified in women since their excretions improve.
According to the Bone Cancer Advocacy Network, women are more likely than men to die from bladder cancer.
The most frequent symptom is racing in the urine, but some women also have a painful, burning feeling while peeing.
Please Read This Great Info chronic-disease-get-habit-under-control
Bladder cancer therapies

include surgery, chemotherapy, radiation therapy, and immunotherapy.
According to the American College of Surgeons (ACS), Bladder cancer treatment , Reproductive system most patients need surgical removal of swelling.
In extreme circumstances, the Bladder cancer treatment is completely or partially removed.
Siddiqui believes it is critical to determine if the uterus and other gynecological organs are causing bladder discomfort since they are so near to the Reproductive system.
Pelvic bottom dysfunction, Bladder cancer treatment, which is related to miserliness or pelvic muscular spasms, is often associated with bladder discomfort and may exacerbate it, she says.
Please Read This Great Info general-adaptation-syndrome-stages
A person with this illness

may also be unable to relax and conciliate these muscles enough to make a bowel movement.
The Cleveland Clinic lists some of the symptoms associated with this condition as being constipation, straining to urinate, pee or coprolite leakage, and a persistent urge to urinate.
Endometriosis, Bladder cancer treatment, pelvic seditious complaints, and ovarian excrescences may all cause pelvic discomfort.
The Mayo Clinic also reports that ulcerative colitis and Bladder cancer treatment are gastrointestinal disorders that may sometimes manifest as pelvic pain.
Nonetheless, they are often treated for bladder pain pattern, which refers to painful bladder diseases after other antecedents such as UTI and cancer have been ruled out.”
If none of these disorders are present and women experience continuous bladder Reproductive system,
The most important sentence for women to remember Do not use tone to identify your Reproductive system discomfort.
Reproductive system –
Addressing and treating the conclusion may provide relief fo